Katie attended a class in Loughborough with Fernanda Salfity, here she share’s the story of her son’s birth. “I would…
Read More
induction
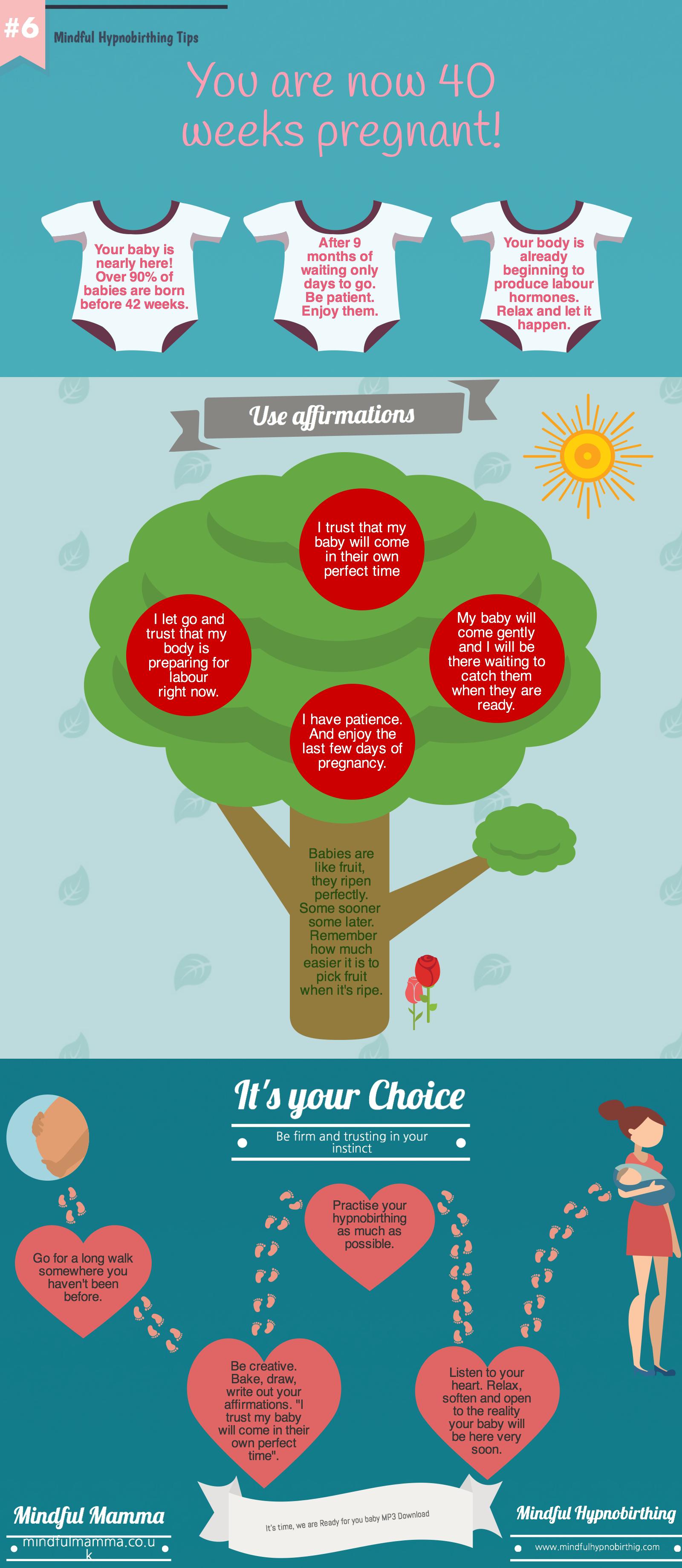
40 Weeks pregnant and counting!
I’m going to be have a labour induction can I use hypnobirthing? Yes!
A Labour Induction and hypnobirthing. I know mums who have had a labour induction because of medical reasons, but I…
Read More
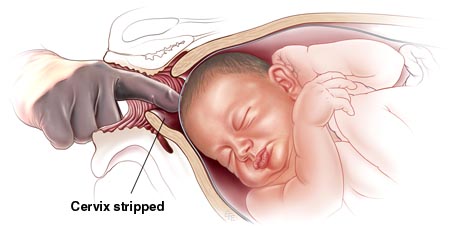
Shall I Have a Membrane Sweep?
Shall I have a Membrane Sweep? A membrane sweep is a common form of intervention that is routinely offered in…
Read More
You pass your due date and it’s “have you had the baby yet?”.
The due date countdown and friends who can’t help asking is the baby is here yet. by Sophie Fletcher “Have…
Read More